Understanding Dental Impression Scanners
2024-07-07
2024-11-10
In the field of restorative dentistry, all-ceramic zirconia is favoured for its excellent aesthetic results and biocompatibility. In this article, we will discuss in depth the key technical points of all-ceramic zirconia tooth preparation and provide you with a comprehensive operational guide.
I. Occlusal surface preparation
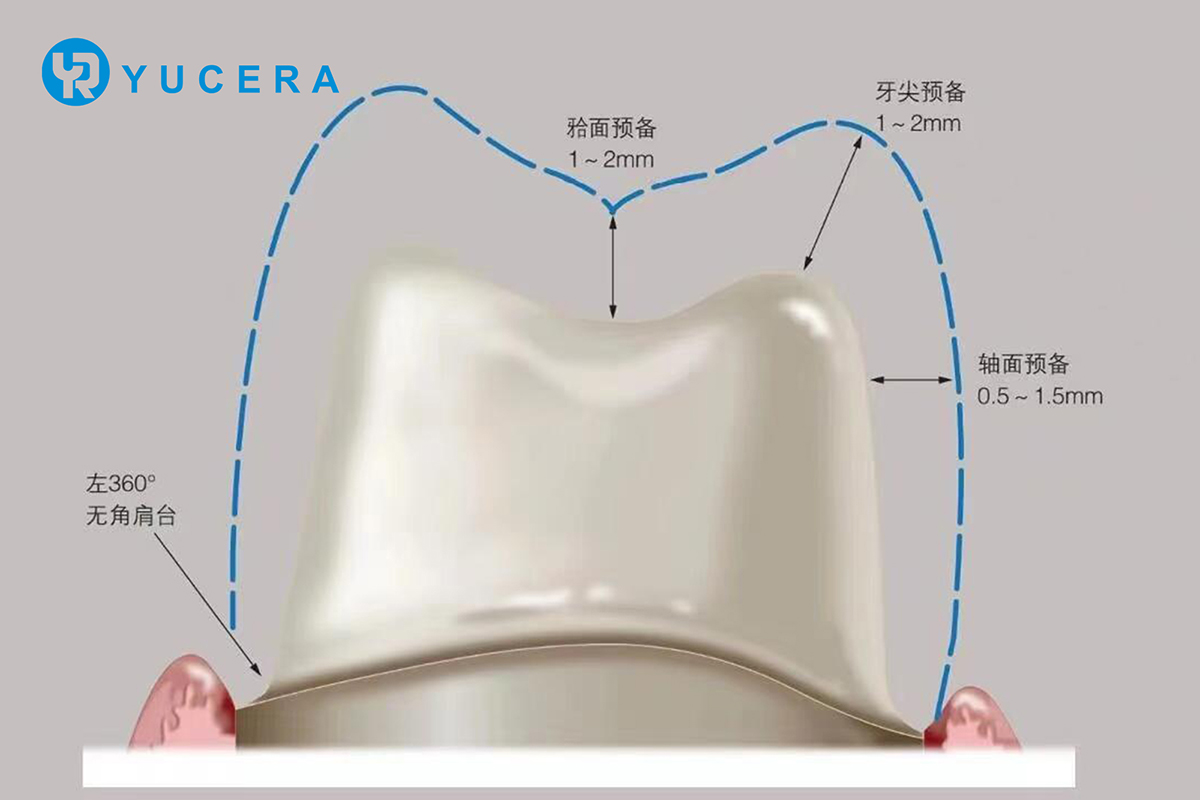
The occlusal thickness of traditional all-ceramic materials used for full crown restoration is generally 1.5-2.0 mm, while the strength of zirconia can reach 800 MPa or more, significantly exceeding that of traditional all-ceramic materials, and its fracture toughness is also much higher, reaching 5-10 MPa-m½. Studies have shown that restorations with plain all-zirconia crowns require at least 0.5 mm of restorative space, and in special cases such as nocturnal grinding or discolouration of the abutment, the amount of tooth preparation should be moderately increased. Therefore, the recommended amount of preparation is 0.5-1.0 mm for plain all-zirconia crowns, and it has been found that anatomical preparations with an apical inclination of 30° are significantly better than semi-anatomical (apical inclination of 15-30°) and non-anatomical preparations (apical inclination of 0°) in terms of margins and internal fit. Therefore, anatomical preparations are preferred for occlusal surfaces.

II. Axial tooth preparation
The total occlusal convergence (TOC) is an important parameter in the preparation of axial dentition, as the TOC decreases, the retention force can be improved. However, due to the high technical sensitivity of the preparation, it is difficult to achieve a TOC value of 2-5° in practice, and it may also increase the hydrostatic pressure of the bonded cementum, which may affect the spillage of excess cementum. Therefore, it is recommended to keep the TOC in the range of 10-22°, and the exact TOC value should depend on the type of abutment. For example, for mandibular first molars, it is generally recommended to set the TOC at 24° in the proximal-distal-medial direction and 22° in the buccolingual direction. The thickness of the axial wall of an all-zirconium crown does not significantly affect the fracture strength, and it is recommended that the thickness of the axial wall of an all-zirconium crown be at least 0.5 mm.
III. Edge design
Porcelain edges made from conventional all-ceramic materials are slightly weaker than metal edges and are more difficult to machine into edge-shaped edges. In clinical practice, all-ceramic crowns are often made with a fluted edge or a shoulder. Nowadays, with the use of zirconia ceramics and the improvement of all-ceramic processing techniques, zirconia crowns with a sharp edge are available. Shoulder tables have a greater fracture load capacity, whereas edgewise and fluted edges help to retain more of the tooth tissue. The fracture load of a fluted margin is related to its depth, and the use of a deep fluted margin design increases the material thickness and results in rounded inner corners and, therefore, higher fracture loads. Flush gingival margins provide superior self-cleaning, less gingival irritation, and more accurate impressions than subgingival margins. Therefore, except for cases where the abutment tooth is missing up to the gingival margin, it is recommended that a flush gingival margin design be preferred.
IV. Ultra-transparent zirconia tooth preparation
Ultra-transparent zirconia is less strong than ordinary zirconia and therefore requires more careful design of the crown thickness. Even a slight increase in thickness can significantly improve strength, and the minimum thickness recommended for clear zirconia crowns is 0.8 mm. For normal-coloured abutments, clear zirconia can be chosen from 0.8 to 1.5 mm. In view of the fact that thinner margins are more prone to fracture, the marginal design of clear zirconia crowns is recommended to be based on a fluted margin or an internally rounded shoulder, with an appropriate increase in width.